We often see lots of bugs and viruses circulating at this time of year and it can be hard to know what the right thing is to do if your child falls ill.
With that in mind, the NHS in Gloucestershire has developed this summary for parents and carers of children to help them know when health advice might be needed and what action to take.
It’s important to mention that there are lots of viruses that cause sore throats, colds and coughs at this time of year. Most are mild, should resolve without medical intervention and can be managed at home with self-care.
Below is some advice about the signs and symptoms to look out for, when you should be fine to keep your child at home with a bit of self-care (which could include some advice from the community pharmacy) and when it’s time to ask for advice or help from another NHS service.
Prevention
Good hand and respiratory hygiene are important for stopping the spread of many bugs.
By teaching your child how to wash their hands properly with soap for 20 seconds, using a tissue to catch coughs and sneezes, and keeping away from others when feeling unwell, they will be able to reduce the risk of picking up or spreading infections.
If you think your child has a common viral infection (e.g. coughs, colds, flu)
For viral infections, there are a few things you can do to look after your child at home without needing to seek medical advice.
If you need it, a community pharmacy is a great first port of call for advice (no appointment required) and they can signpost on to other NHS services if needed.
Here are some self-care pointers:
- You may want to give your child paracetamol (e.g. calpol) and/or ibuprofen. This not only helps with fever but also reduces pain.
- Give your child plenty of drinks e.g. water or squash. If you are breastfeeding then continue to do so. Give babies smaller but more frequent feeds to keep them hydrated.
- Do not worry about food if your child does not feel like eating for a while, but encourage them to drink more fluids.
- Children with a fever should not be over or underdressed. If your child is shivering or sweating a lot, change the amount of clothes they are wearing.
- Physical methods of cooling your child such as fanning them, cold bathing and tepid sponging can cause discomfort and are not advised.
- Check on your child regularly, including during the night, especially if your child is under 6 months old as they are at higher risk of serious infection.
- Keep your child away from nursery or school whilst they have a fever.
When to get further advice or help
Contact NHS 111 or your GP if:
- you suspect your child has measles so they can be assessed for treatment (see section below)
- your child has a fever for more than 5 days and doesn’t seem to be getting any better
- your child is drinking much less than normal · your child has had a dry nappy for 12 hours or more or shows other signs of dehydration
- your baby is under 3 months and has a temperature of 38°C, or is between 3 and 6 months and has a temperature of 39°C or higher
- your child is drowsy (much more sleepy than normal) or irritable (unable to settle them with cuddles, toys, TV or snacks – especially if they remain drowsy or irritable despite any fever coming down)
Call 999 if:
- your child is having difficulty breathing – you may notice grunting noises or their tummy sucking under their ribs
- there are pauses when your child breathes
- your child’s skin, tongue or lips are blue
- your child is floppy and will not wake up or stay awake.
An increase in measles infections
There’s been a lot of media coverage about a measles outbreak in the West Midlands, where children under the age of ten have fallen ill. We know this is concerning and want to reassure parents that measles is still relatively rare.
However, it can spread quickly, and although it is mild in most cases it can make some children and adults very poorly. In rare cases people with measles will need hospital treatment.
One of the reasons we are seeing more cases of measles across the country is due to far fewer children having both doses of the vaccination against measles, mumps and rubella (MMR).
We know the pandemic and other factors mean some children have not been able to have both doses. We want to remind parents and carers that it is never too late to protect you and your child with the vaccine. You can find out more about how to check your child’s vaccination status and arrange catch up doses here .
How do you know if its Measles?
Early signs of measles can include a runny nose, fever or cough, but these are common to lots of winter bugs. It’s very unlikely to be measles if your child has had both doses of the MMR vaccine or had measles before. If not fully vaccinated, measles is still very rare.
In cases of measles, children will develop a rash within a few days of starting to feel poorly. Some people may also get small spots in their mouth.
If your child develops a rash (see photos below), contact your GP surgery or get advice from NHS 111. Your GP may suggest talking over the phone, because measles can spread easily.
After consultation with your GP, there are things you can do to help ease the symptoms and reduce the risk of spreading the infection.
It can help to follow the self-care advice above, but also use cotton wool soaked in warm water to gently remove any crusts from your child’s eyes.
 |
Small white spots may appear inside the cheeks and on the back of the lips a few days later. These spots usually last a few days. |
 |
A measles rash usually appears a few days after the cold-like symptoms. The rash starts on the face and behind the ears before spreading to the rest of the body. |
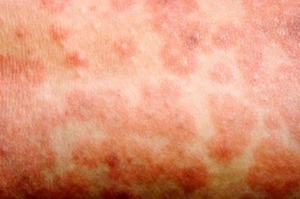 |
The spots of the measles rash are sometimes raised and join together to form blotchy patches. They’re not usually itchy. |
|
|
The rash looks brown or red on white skin. It may be harder to see on brown and black skin. |
Important
Stay off nursery, school or work for at least 4 days from when the rash first appears.
Also try to avoid close contact with babies and anyone who is pregnant or has a weakened immune system.



